Eco-label Raises Questions
By gofb-adm on Wednesday, September 29th, 2021 in Issue 3 - 2021, Nutrition No Comments

By gofb-adm on Wednesday, September 29th, 2021 in Issue 3 - 2021, Nutrition No Comments
In March and April, respectively, retailers Colruyt in Belgium and Lidl in Germany announced the implementation of Eco-Score, a new front-of-pack (FoP) labelling scheme for some of their products. The label aims at indicating the environmental impact of food products in a simplified way.
Eco-Score looks very similar to Nutri-Score, a widely known voluntary FoP nutrition label. Eco-Score was developed in France by the ECO2 Initiative, a consulting firm focusing on environmental transition. The method for calculating the Eco-Score consists of two components:
These elements are converted by the system’s algorithm into a code for a food product consisting of one of five letters of the alphabet, each with a colour – from A (green) for the lowest environmental impact of a product, to E (red) for the highest environmental impact.
On its part, Nutri-Score is a colour-coded system that rates the nutritional value of a food product by assessing the content of key nutrients: salt, fat, saturated fat, sugar and total calorie count. Unlike the ‘traffic light’ label, which highlights key individual nutrients, the Nutri-Score system – introduced in France in 2017 – provides a single score for the entire product, giving consumers an overall assessment of the product.
Based on an algorithm, Nutri-Score gives a rating to any food except single-ingredient foods and water. The rating ranges from dark green A (best) to red E (worst), by weighing the prevalence of ‘good’ and ‘bad’ nutrients.
For both Nutri-Score and Eco-Score, the very idea of a ‘score’ means that they cannot convey any specific information to the consumer on the actual nutritional properties or the specific environmental impact. Notably, these schemes have outpaced ongoing developments at the EU level.
On May 20, 2020, the European Commission (EC) adopted its Farm to Fork (F2F) strategy for a fair, healthy and environmentally-friendly food system, as part of the European Green Deal.
The strategy announced that, in order to promote sustainable food consumption and facilitate the shift to healthy and sustainable diets, the EC would adopt measures to empower consumers to make informed, healthy and sustainable food choices. In particular, the strategy announced that the EC would propose a harmonised mandatory FoP nutrition labelling.
In relation to environmental labels, the F2F strategy announced that the EC would ‘also examine ways to harmonise voluntary green claims and to create a sustainable labelling framework that covers, in synergy with other relevant initiatives, the nutritional, climate, environmental and social aspects of food products’.
Evolving legal framework
The main question related to claims on food products is how they are substantiated. This concerns claims about nutritional, health or environmental properties. Unlike for nutrition and health claims under Regulation (EC) No. 1924/2006 on nutrition and health claims made on foods, there is currently no specific legal framework in the EU on the substantiation of environmental labels or claims.
Competent authorities in the EU member-states can prohibit environmental claims that they find to be misleading towards consumers on the basis of a case-by-case application of existing consumer protection laws.
In particular, the laws are:
The EC is currently preparing a legislative proposal on ‘substantiating green claims’. The related Inception Impact Assessment (i.e. Roadmap) notes that it concerns ‘claims made in relation with the environmental impacts covered by the Environmental Footprint methods’.
According to the Product Environmental Footprint Initiative, these methods measure the environmental performance of a product throughout the value chain, from the extraction of raw materials to the end of life, using a large variety of categories: ‘Some of them are focused on a single issue, e.g. carbon footprint, whereas some encompass multiple environmental themes.’
The Roadmap points out that, ‘in order not to mislead, environmental claims should be presented in a clear, specific, unambiguous and accurate manner’. The initiative aims to ‘make the claims reliable, comparable and verifiable across the EU – reducing greenwashing (companies giving a false impression of their environmental impact)’. This, in turn, ‘should help commercial buyers and investors make more sustainable decisions and increase consumer confidence in green labels and information’.
According to the EC, a proposal for a regulation on green claims was planned for the second quarter of this year. However, it appears that the proposal has been delayed and will only be published during the second semester of this year. A proposal for a directive on consumer empowerment for the green transition that aims at establishing specific rules to combat greenwashing was similarly expected in the second quarter, but will now likely only be published during the second half of this year.
Mandatory scheme?
Alongside the F2F strategy, the EC published a Report to the European Parliament and the Council regarding the use of additional forms of expression and presentation of the nutrition declaration (FoP Report). This included a reference to schemes providing information on the ‘overall nutritional quality of foods’, such as the Nutri-Score scheme, which has been introduced in various EU member-states.
The FoP Report states that, given the political priority of the F2F strategy – namely the potential of FoP schemes enabling consumers to make health-conscious food choices – ‘it seems appropriate to introduce a legislative proposal on a harmonised mandatory FoP nutrition labelling scheme at EU level’.
In the F2F strategy, the EC announced that, by the fourth quarter of 2022, after launching an impact assessment on the different types of FoP schemes, it intends to prepare such legislative proposal on harmonised mandatory FoP nutrition labelling.
No specific scheme has been recommended in the FoP Report. It appears that schemes providing information on the FoP on the overall nutritional quality of foods, such as the Nutri-Score, do not appear to be appropriate for a harmonised mandatory nutrition labelling scheme under the current legal framework of Regulation (EU) No. 1169/2011 of the European Parliament and of the Council of Oct 25, 2011, on the provision of food information to consumers (FIR).
In particular, they arguably fall short of complying with Article 35(1) of the FIR According to this, the mandatory nutrition declaration may be complemented by a voluntary repetition of the energy value and the amount of nutrients in the principal field of vision (also known as the FoP), in order to help consumers see at a glance the essential nutrition information when purchasing foods. Nutri-Score does not provide for such a repetition of the energy value and the amount of nutrients.
Setting of nutrient profiles
The FoP Report also includes a reference to nutrient profiles. According to the World Health Organisation, nutrient profiling is the categorisation of foods according to their nutritional composition using predefined criteria. Nutrient profiles have a variety of applications around the world, for example, for purposes of regulating food marketing to children.
Nutrient profiling is also commonly used in FoP nutrition labelling schemes. Regulation (EC) No. 1924/2006 on nutrition and health claims made on foods requires the EC to adopt nutrient profiles. According to the F2F strategy, the setting of nutrient profiles to restrict the promotion of foods that are high in fat, sugar and/or salt and to stimulate sustainable food processing and reformulation, is foreseen for the fourth quarter of 2022. Nutrient profiles and their categorisation of foods according to their nutritional composition could also become relevant in determining the ‘overall nutritional quality of food’.
There is no doubt that nutrition labels must be based on science. On Dec 14, 2020, in accordance with Article 29(1)(a) of Regulation (EC) No. 178/2002 of the European Parliament and of the Council of Jan 28, 2002 – laying down the general principles and requirements of food law; establishing the European Food Safety Authority (EFSA); and laying down procedures in matters of food safety – the EC requested the EFSA to provide scientific advice for the development of harmonised mandatory FoP nutrition labelling and the setting of nutrient profiles for restricting nutrition and health claims on foods.
In particular, the EFSA was requested to provide scientific advice on the following:
The EFSA has accepted the proposed deadline and expects to deliver its scientific advice by March 31, 2022. In this context, the EFSA will hold a public consultation on its draft scientific opinion.
The food industry now awaits the EC’s proposal for a regulation on the substantiation of green claims and a proposal for a directive on consumer empowerment for the green transition for 2021. The EC also intends to prepare a legislative proposal on harmonised mandatory FoP nutrition labelling by the fourth quarter of 2022. But in the meantime, schemes like Eco-Score and Nutri-Score are spreading around the EU.
Supporters of Nutri-Score and Eco-Score claim to be transparent and to strictly take into consideration scientific criteria – on nutritional aspects for Nutri-Score and on the environmental impact for Eco-Score. However, these schemes are also criticised as being mere marketing tools.
“A system similar to Nutri-Score for environmental aspects would create more confusion and would be equally misleading as it would be intended not to inform consumers but to tell them what to buy,” a spokesperson of the No-Nutriscore Alliance stated.
Notably, an official of the EU has publicly denounced the “ideological fallacy in describing the Nutri-Score as a panacea”.
In light of all this, it is important for the EU to establish a legal framework requiring companies making green claims to substantiate them. The same should apply to nutrition labels, which should inform and educate consumers rather than simply influence their purchasing decisions. Stakeholders in the agri-food sector should carefully observe both initiatives, taking action to ensure that their legitimate interests are voiced and represented within all relevant fora.
FratiniVergano’s Trade Perspectives©
By gofb-adm on Monday, June 24th, 2019 in Issue 2 - 2019, Nutrition No Comments
The well-known tagline:
“Saturated fats cause heart diseases”
“Palm oil is a saturated fat”.
These smear campaigns are aimed at demonising tropical oils and specifically palm oil. The negative labelling had badly affected and stigmatised palm oil. This is a ploy used by the competitor to hide the harmful health problems caused by trans fats or “artificial saturated fats” they had produced, and through deceitful marketing, portrayed it as a natural saturated fat issue (https://experiencelife.com/article/big-fat-controversy/). Based on a report published in the American Journal of Preventive Medicine, Time magazine mentioned that Denmark had banned trans fats between 2003 and 2012, resulting in deaths caused by cardiovascular disease to slide from 359.9 to 210.9 per 100000 people (http://time.com/4025570/denmark-trans-fat-ban/). US FDA (Food and Drug Administration) ban only starts in 2018 (https://www.nytimes.com/2015/06/17/health/fda-gives-food-industry-three-years-eliminate-trans-fats.html).
Ancel Keys first hypothesise that dietary saturated fat causes cardiovascular heart disease and should be avoided (https://en.wikipedia.org/wiki/Ancel_Keys). In 1957, he and his colleagues embarked on an intensive survey comprising 12 000 men aged from 40 to 59 from 18 regions of seven countries and is known as the “Seven Countries Study”. The report published in 1970 had a decisive impact on cardiovascular disease (CVD) prevention, as it described one of the first studies to clearly show that dietary saturated fat leads to CVD, and that the relationship is mediated by serum cholesterol (https://www.bcmj.org/articles/ancel-keys-and-lipid-hypothesis-early-breakthroughs-current-management-dyslipidemia). A physiologist by training, Ancel Keys also ended up in the nutrition committee of the American Heart Association (AHA). In 1961, AHA endorsed Ancel’s hypothesis as a dietary guideline (https://www.wsj.com/articles/the-questionable-link-between-saturated-fat-and-heart-disease-1399070926). On 15 June 2017, AHA’s presidential address once again called for saturated fats to be replaced by polyunsaturated and monounsaturated fats (http://circ.ahajournals.org/content/early/2017/06/15/CIR.0000000000000510). Mr Taubes, an investigative science journalist, found AHA cherry-picked and use severely deficient data to support their stand on saturated fats. He also proved beyond a reasonable doubt, that the evidence against saturated fat is inconsistent, weak, and unreliable (http://www.cardiobrief.org/2017/06/21/my-beef-with-the-ahas-saturated-fat-recommendations/). To add salt to saturated fats’ wound, the sugar industry secretly paid three Harvard scientists to shift the heart diseases and sugar link and blamed it on saturated fats (https://www. nytimes.com/2016/09/13/well/eat/how-the-sugar-industry-shifted-blame-to-fat.html).
Lately, using meta-analysis, a statistical method that combines many separate but similar studies and pool the data to develop a single conclusion, has shown that saturated fat is not linked to heart diseases (http://www.cam.ac.uk/research/ news/new-evidence-raises-questions-about-the-link-between-fatty-acids-and-heart-disease;https://fhs.mcmaster.ca/qa/network/fats.html; http://www.bmj.com/content/351/bmj.h3978). The US Dietary Guidelines Advisory Committee is withdrawing its warning on cholesterol, and hopefully saturated fats will follow suit, as it was reported that subsequent studies have failed to confirm saturated fats and heart diseases risk (https://www.aocs.org/stay-informed/read-inform/featured-articles/big-fat-controversy-changing-opinions-about-saturated-fats-june-2015). Before going into detail, it is necessary to understand the relevant terms used and their meaning.
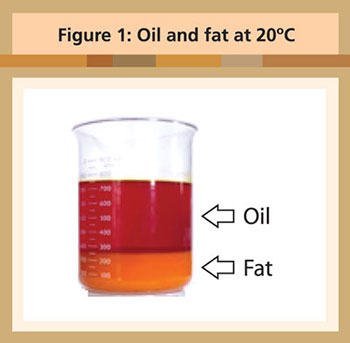
The term oil and fat are often used interchangeably to mean the same thing. Strictly speaking, there is a difference. At 20ºC, oil is liquid, and fat is solid (Figure 1). Palm oil is unique as it has natural fractions of both oil and fat. The ratio of oil (olein) to fat (stearin) production in 2005 in Malaysia was 3.5-to1 (http://bepi.mpob.gov.my/news/detail.php?id=3045). This makes palm oil highly versatile and can be used in a lot of applications, be it food or non-food!
TYPES OF OILS AND FATS: THE TRAIN ANALOGY
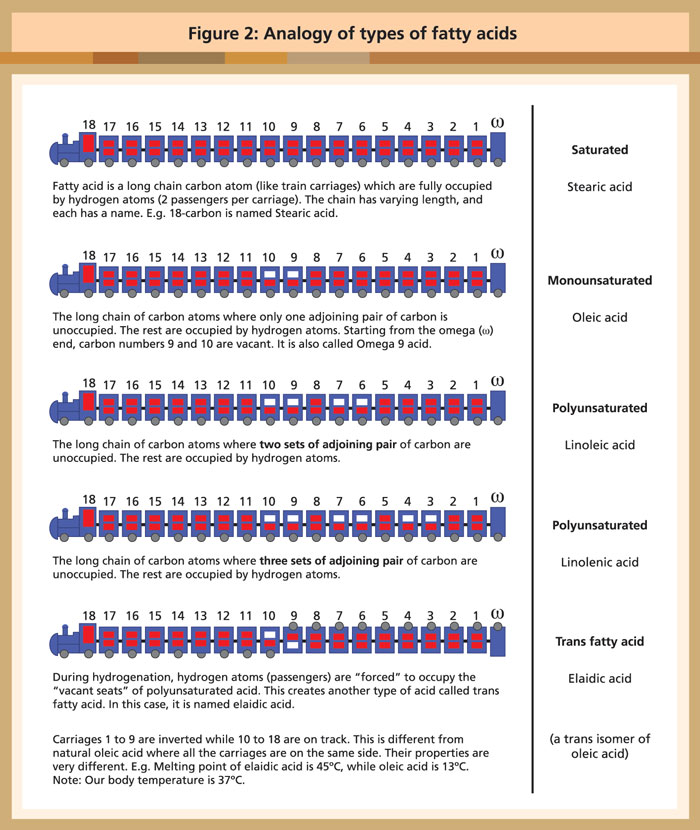
The properties of the oils and fats are largely governed by the types of fatty acids present.
These fatty acids are further grouped together based on the number of vacant spaces within each acid.
To illustrate, think of a fatty acid as a train with a range of carriages. In each carriage, there are two vacant seats. If the seats in all the carriages are taken, the train is said to be saturated. If one seat each in the adjoining carriage is vacant, it is said to be monounsaturated. Likewise, two or more seats in the adjoining carriages are vacant, it is termed as polyunsaturated.
Polyunsaturated oils are very unstable. They have poor shelf life, which means the oil that is produced cannot be kept for long before turning bad (rancid). Such oil cannot be used for frying or for making solid products such as cakes, biscuits or pastries unless they are hydrogenated. Going back to the train analogy, hydrogenation process is like “forcing passengers to occupy the vacant seats” to stabilise it. In other words, it is an “artificial way to saturate” the oil. The hydrogenation process also creates another type of acid called trans fatty acid, which is a twisted form of the natural oleic acid. The analogy of the types of fatty acids are as sketched in Figure 2.
IS PALM OIL SATURATED OR UNSATURATED?
This is best answered by referring to Malaysian Standard, MS814:2007. The fatty acid composition for palm oil is as quoted in Table 1 (Adapted from Malaysian Standard, MS814:2007). The overall composition is:
| Palm oil | Mean |
| Saturated | 49.3% |
| Unsaturated | 50.6% |
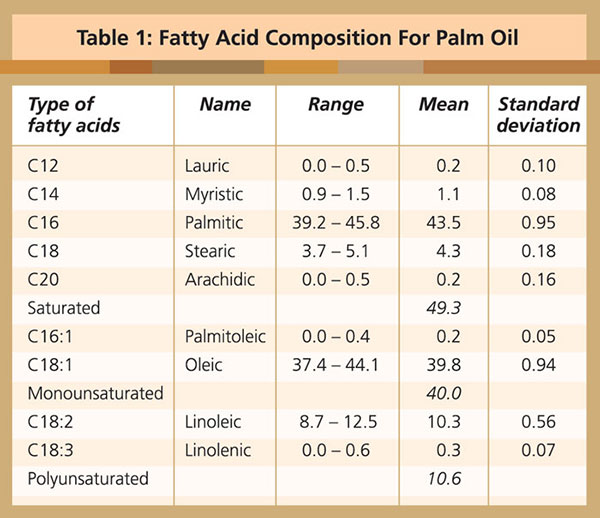
The points to note are:
• The arithmetic mean shows that palm oil is more than 50 per cent unsaturated. By a simple majority rule, palm oil is “unsaturated”. It is wrong to label palm oil as “saturated”.
• Apart from having natural liquid and solid fractions, there is another feature about palm oil, it naturally has nearly equal saturated and unsaturated portions.
This is a classic case of the proverbial “half empty or half full glass of water” expression. How one interprets it depends on one’s state of mind and intention. This is best defined by the Cambridge dictionary, which says:
“The glass is half empty” refers to an attitude of always thinking about the bad things in a situation rather than the good ones.
As evident from the above-mentioned, palm oil has more oil than fat and it is slightly more unsaturated than saturated. Based on these facts, palm oil should be labelled as an “unsaturated oil”. One can only surmise that whoever that labelled palm oil as a “saturated fat” choose to disregard or distort the facts because of ulterior motives.
SATURATED FAT AND HEART DISEASE
In the 1950s, heart disease was America’s number one killer and when President Eisenhower had a heart attack in 1955, there was a desperate need for answers (https://www.wsj.com/articles/the-questionable-link-between-saturated-fat-and-heart-disease-1399070926). It was Ancel Keys who hypothesised that dietary saturated fat causes cardiovascular heart disease and should be avoided (https://en.wikipedia.org/wiki/Ancel_Keys). The suggestion, as can be expected, was readily accepted.
In 1958, Keys’s subsequent observational “Seven Countries Study” demonstrated heart disease could be linked to poor nutrition. Keys, a physiologist, also ended up on the nutrition committee of AHA. In 1961, AHA issued the country’s first ever guidelines targeting saturated fat (https://www.wsj.com/articles/the-questionable-link-between-saturated-fat-and-heart-disease-1399070926). The guidelines had remained unchanged for many decades. On 15 June 2017, AHA’s stand was reaffirmed via its presidential address, which concluded that based on evidence, called for a reduction in saturated fat and replace it with polyunsaturated and monounsaturated fat (http://circ.ahajournals.org/content/early/2017/06/15/CIR.0000000000000510).
American Heart Association cherry picking data on saturated fats
Mr Gary Taubes, an award-winning science writer, author and a prominent investigative journalist took AHA to task in a post published by Cardio Brief, a source for new and important information about cardiovascular medicine.
AHA pretends to be science-based but is not. There is no strong scientific basis to support their guidelines but are opinions. Their recommendation that saturated fats be replaced with polyunsaturated fats, is based on cherry-picked and severely deficient data. With the devastating precision of a prosecuting attorney, Taubes lays out the case against the AHA paper. He doesn’t prove that saturated fat is innocent, but that’s not his goal. He does prove, beyond a reasonable doubt, that the evidence against saturated fat is inconsistent, weak, and unreliable. “If the data doesn’t exist, you must acquit,”I suppose he might say (http://www.cardiobrief.org/2017/06/21/my-beef-with-the-ahas-saturated-fat-recommendations/)
Taubes, was also quoted in Olive Health News, said “The AHA ignores results from some of the biggest studies ever conducted, including the Minnesota Coronary Survey, Sydney Heart Study and the Women’s Health Initiative” (https://www.oliveoiltimes.com/olive-oil-health-news/experts-dispute-aha-warning-saturated- fats-coconut-oil/58005).
One such example is the Sydney Heart Study quoted below.
Sydney (Diet) Heart study
In this cohort, substituting dietary linoleic acid (a polyunsaturated acid) in place of saturated fats increased the rates of death from all causes, coronary heart disease, and cardiovascular disease. An updated meta-analysis of linoleic acid intervention trials showed no evidence of cardiovascular benefit. These findings could have important implications for worldwide dietary advice to substitute omega 6 linoleic acid, or polyunsaturated fats in general, for saturated fats (http://www.bmj.com/content/346/bmj.e8707). These results clearly contradict AHA’s guidelines and as Mr Taubes quite rightly said, the results were ignored.
Nutritional policy: Personal ambition, bad science, politics and bias
Wall Street Journal also ran an article by Nina Teicholz, another investigative journalist and author of the International (and New York Times) bestseller, The Big Fat Surprise. She too questioned the saturated fat link. The nutritional policy, she writes, had been derailed over the past half-century by a mixture of personal ambition, bad science, politics and bias.
She added that there is no solid evidence to back up the idea that saturated fats cause disease. Critics have pointed out that Dr Keys violated several basic scientific norms in his study. For one, he did not choose countries randomly but instead selected only those likely to prove his beliefs, including Yugoslavia, Finland and Italy (https://www.wsj.com/articles/the-questionable-link-between-saturated-fat-and-heart-disease-1399070926). Keys’s original studies covered twenty-two countries out of which only seven countries were chosen.
Saturated fat and heart disease: A questionable link
In the last four years, two meta-analysis studies on saturated fats were published in reputable journals are mentioned below. Also included is a diet intervention study from Norway. Meta-analysis is a method for systematically combining pertinent qualitative and quantitative study data from several selected studies to develop a single conclusion that has greater statistical power (https://en.wikipedia.org/wiki/Meta-analysis).
In June 2015, American Oil Chemists Society (AOCS) reported a promising sign that the US Dietary Guidelines Advisory Committee is withdrawing its warning on cholesterol. Perhaps saturated fats will follow suit. These main points were extracted from an article in AOCS’s publication.
AOCS: Big fat controversy – Changing opinions about saturated fats
Nutritionists have long vilified saturated fat for its propensity to raise LDL (“bad”) cholesterol levels in the blood. Although initial epidemiological studies associated saturated fat intake with heart disease risk, subsequent studies have failed to confirm the link. Saturated fat raises HDL (“good”) cholesterol levels, perhaps ameliorating its effects on LDL cholesterol. An unintended consequence of a low-fat diet may be increased carbohydrate intake, which could actually raise heart disease risk compared to a higher-fat diet (https://www.aocs.org/stay-informed/read-inform/featured-articles/big-fat-controversy-changing-opinions-about-saturated-fats-june-2015).
Not all saturated fats are the same
A closer look at only the saturated fatty acids components of both animals and vegetable oils may help us understand the situation better (Table 2).
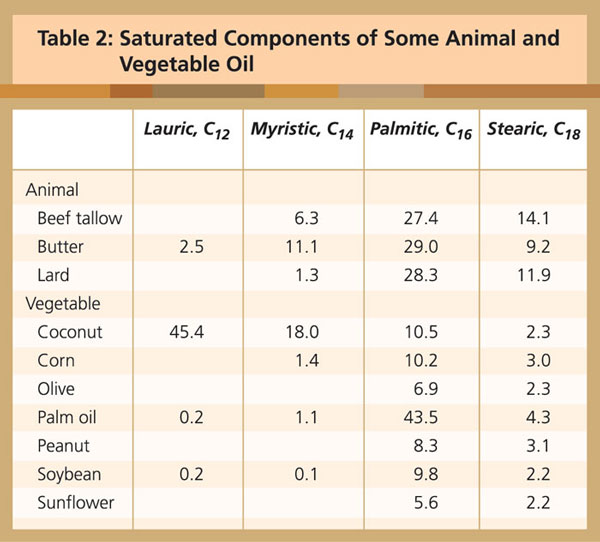
In palm oil, the predominant saturated acid is palmitic acid, and, to a lesser extent, stearic acid. The Cambridge team concluded:
Palm oil, the fall guy
The saturated fat mentioned so far referred mainly to red meat and dairy products. AHA’s recommendation is to switch to polyunsaturated vegetable oils, namely corn, soybean and canola. These oils require hydrogenation to mimic saturated oil. When health problems related to trans fats arose, labelling tropical oils as “saturated fat” fits the bill as no distinction is made between artificial or natural saturated fat. This made palm oil the main fall guy.
THE REAL HEALTH CULPRIT IS TRANS FATS
Dr Mary Enig, an internationally renowned nutritionist and lipids biochemist, is known for her unconventional positions on the role saturated fats play in diet and health. Her views appeared in “The big fat controversy” (https://experiencelife.com/article/big-fat-controversy).
The real health culprit is not saturated fats but rather trans fats, which were introduced into the food supply in great quantity by the soy industry in the 1950s. This is when partially hydrogenated fats were developed to imitate naturally saturated fats and to expedite the production of processed foods.
To create the solid substance, manufacturers typically take vegetable fats and bombard them with hydrogen, turning them into the solids used in commercial baked goods or to make shortening from vegetable oil. “They have a different shaping than the normal kind of fatty acids that are in the food supply or in the tissues of the body,” Enig says. “Trans fats also have a higher melting point, all of which can make them very harmful to the system.”
The food industry has so cleverly marketed these trans fats, insists Enig, and so regularly bad-mouthed saturated fats, that in the last 30 years their dogma has been accepted as gospel by the medical establishment – and, by extension, the general public, which is why low-fat, processed foods are so prevalent and popular these days.
Trans fats are deadly
Consumption of industrial trans fats was associated with a 34 per cent increase in death for any reason (https://fhs.mcmaster.ca/qa/network/fats.html; http://www.bmj.com/content/351/bmj.h3978). Time magazine carried an article that Denmark’s trans-fat ban in 2004 worked based on an article published in the American Journal of Preventive Medicine on 9 September 2015. Between 2003 and 2012, deaths caused by cardiovascular disease slid from 359.9 to 210.9 per 100 000 people, a 9-point drop. Between 2004 and 2006, cardiovascular disease mortality rates dropped by 4 per cent – the equivalent to 750 fewer deaths per year in that period (http://time.com/4025570/denmark-trans-fat-ban/).
On 16 June 2015, the US Food and Drug Administration gave the food industry three years to eliminate artery-clogging artificial trans fats from the food supply, a long-awaited step that capped years of effort by consumer groups and is expected to save thousands of lives a year (https://www.nytimes.com/2015/06/17/health/fda-gives-food-industry-three-years-eliminate-trans-fats.html). On 14 August 2015, in the British Medical Journal, experts from Oxford and Liverpool Universities suggested that banning trans fats from processed foods could save around 7 200 deaths from heart disease in England over the next five years (http://www.bmj.com/content/351/bmj.h4583). In Malaysia, popular commercial pastry shortening samples were found to contain up to 34.4 per cent trans fats (http://palmoilis.mpob.gov.my/publications/TOT/TT540.pdf).
HARVARD SCIENTISTS PAID TO SHIFT BLAME FROM SUGAR TO SATURATED FAT
The Journal of the American Medical Association (JAMA) dropped the bombshell by reporting that the sugar industry paid scientists to shift blame on saturated fat. This was picked up by various newspapers and excerpts from The New York Times on 12 September 2016 (https://www.nytimes.com/2016/09/13/well/eat/how-the-sugar-industry-shifted-blame-to-fat.html).
The sugar industry paid scientists in the 1960s to play down the link between sugar and heart disease and promote saturated fat as the culprit instead, newly released historical documents show.
The internal sugar industry documents, recently discovered by a researcher at the University of California, San Francisco, and published in JAMA Internal Medicine, suggest that five decades of research into the role of nutrition and heart disease, including many of today’s dietary recommendations, may have been largely shaped by the sugar industry.
“They were able to derail the discussion about sugar for decades,” said Stanton Glantz, a professor of medicine at U.C.S.F. and an author of the JAMA Internal Medicine paper.
The documents show that a trade group called the Sugar Research Foundation, known today as the Sugar Association, paid three Harvard scientists the equivalent of about $50,000 in today’s dollars to publish a 1967 review of research on sugar, fat and heart disease. The studies used in the review were handpicked by the sugar group, and the article, which was published in the prestigious New England Journal of Medicine, minimized the link between sugar and heart health and cast aspersions on the role of saturated fat.
Even though the influence-peddling revealed in the documents dates back nearly 50 years, more recent reports show that the food industry has continued to influence nutrition science.

CONCLUSION
Palm oil is a good oil. It is tainted by unscrupulous competitors in a non-level oils and fats playing field. Currently, there is an outstanding issue of 3 MCPD, a suspected carcinogen to be managed. Palm oil is non-GMO and is mechanically extracted. This is a very strong plus point which will give the oil an edge over its competitors – oilseeds that are mainly solvent extracted. Palm oil extraction efficiency is about 92 per cent compared to around 98 per cent with solvent. Preventing remnant oil recovered from being added back into the system to increase oil extraction is the first step in preventing 3 MCPD. As consumers ourselves, we must adhere to the universal rule: “Food safety must precede profits”, failing which, we are no better than the manufacturers of trans fats!
Ng Say Bock & Vincent Ng
Source: The Planter, Kuala Lumpur, 94 (1103): 79-88 (2018)
This article is reproduced with permission of ‘The Planter’ and the Incorporated Society of Planters.
By gofb-adm on Sunday, December 30th, 2018 in Issue 4 - 2018, Nutrition No Comments
On Oct 4, 2018, the European Commission (EC) published a draft Commission Regulation amending Annex III to Regulation (EC) No 1925/2006 of the European Parliament and of the Council with regard to trans fats, other than trans fats naturally occurring in animal fat, in foods intended for the final consumer. Stakeholders were invited to submit their comments.
The Draft Regulation proposes a maximum limit of trans fats, other than those naturally occurring in animal fat, in food which is intended for the final consumer, of 2g per 100g of fat. Food which does not comply may continue to be placed on the market until April 1, 2021
Trans fats are a particular type of unsaturated fatty acids. In Regulation (EU) No 1169/2011 they are defined as ‘fatty acids with at least one non-conjugated (namely interrupted by at least one methylene group) carbon-carbon double bond in the trans configuration’.
Some trans fats are produced industrially. The primary dietary source of industrial trans fats is partially hydrogenated oils. These generally contain saturated and unsaturated fats, among them trans fats in variable proportions (ranging up to more than 50%), according to the production technology used. Trans fats can also be naturally present in food products derived from ruminant animals, such as dairy products or meat from cattle, sheep or goat.

Timeline and details
Article 1
The following conditions shall apply:
Article 2
– This Regulation shall enter into force on the 20th day following that of its publication in the Official Journal of the European Union.
– Food which does not comply with this Regulation may continue to be placed on the market until April 1, 2021.
– This Regulation shall be binding in its entirety and directly applicable in all member-states.

By gofb-adm on Wednesday, June 21st, 2017 in Issue 2 - 2017, Nutrition No Comments
Health Canada, the governmental health department, has introduced a regulatory proposal to prohibit the use of partially hydrogenated oils (PHOs), the main source of industrially produced trans fats in food.
Read more »By GOFB on Saturday, December 3rd, 2016 in Issue 4 - 2016, Nutrition No Comments
Oils and fats provide about 9 kcal/g of metabolisable energy compared to 4 kcal/g from protein or carbohydrates. In addition to their caloric and nutritional value, oils and fats carry, enhance and release the flavours of other foods, as well as increase palatability. Oils and fats are a good carrier of Vitamins A, D, E and K with excellent bioavailability.
Polyunsaturated fatty acids (PUFA) cannot be synthesised in the body; therefore, oils and fats provide an excellent source of these essential fatty acids (EFA). Saturated and monounsaturated fatty acids are also very important for several vital functions of the body.
For these reasons, oils and fats and different types of fatty acids should now be considered key nutrients that affect early growth and development, as well as nutrition-related chronic diseases later in life.
Oils and fats are structural bodily components; they are involved in vital physiological processes, including growth, development, inflammation and brain function. Combinations of lipid and protein (lipoproteins) are important cellular constituents, occurring both in the cell membrane and in the mitochondria, and further serve as a means of transporting lipids in the blood.
Globally, the nine major oils consumed are palm, soybean, rapeseed, sunflower, peanut, palm kernel, cottonseed, coconut and olive oils. Various other oils and fats are also consumed depending on local priorities and availability. All the dietary oils and fats are composed of a mix of polyunsaturated, monounsaturated and saturated fatty acids.

Omega-6 and Omega-3 fatty acids are essential fatty acids commonly known as PUFA; their deficiency may cause several health problems like cardiovascular disease, diabetes, cancer and age-related functional decline.
High amounts of Omega-6 fatty acids, namely linoleic acid (LA), are present in corn, soybean, sunflower, safflower, cottonseed and sesame oils among others. Omega-3 fatty acids, namely linolenic acid (LnA), are found in select sources like flax seed, soybean and mustard oils.
Fish oil is a unique source of long chain Omega-3 fatty acids, namely eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Over the last decade, some algal oils have been produced as a source of EPA and DHA.
EFAs, namely LA and LnA, are involved in many physiological processes and vital functions such as blood clotting, wound healing and inflammation; they also convert to longer chain fatty acids like arachidonic acid, EPA and DHA. They are further converted to compounds such as prostaglandins, thromboxanes, lipoxin, resolvins and leukotrienes, with hormone-like or inflammatory properties.
PUFA are known for lowering blood total and LDL-cholesterol and slightly increasing HDL-cholesterol. Monounsaturated fatty acids (MUFA) are found in olive, canola, peanut, rice bran, mustard, high oleic sunflower and soybean oils, and are part of animal fats such as chicken, pork and beef. MUFA have a blood total and LDL-cholesterol-lowering effect.
Saturated fatty acids (SFA) are found in the greatest amounts in palm, coconut and palm kernel oils, as well as in cocoa butter, butter and animal fats like beef, pork and chicken. SFA increase blood total, LDL-cholesterol and HDL-cholesterol concentrations and decrease fasting triglyceride concentrations.
By GOFB on Friday, September 30th, 2016 in Issue 3 - 2016, Nutrition No Comments
Debate about food and health is never-ending, as different diets, theories and speculation abound. The only way to test hypotheses is to study them rigorously.
Read more »By GOFB on Friday, September 30th, 2016 in Issue 3 - 2016, Nutrition No Comments
According to the World Health Organisation (WHO), obesity worldwide has more than doubled since 1980. In 2014, over 1.9 billion adults (18 years and older) were overweight – 600 million of them were obese.
Read more »By GOFB on Sunday, July 17th, 2016 in Issue 2 - 2016, Nutrition No Comments
Recent policy changes in Argentina have helped energise many sectors of the agricultural economy. In addition to a lowering in the exchange rate and ending restrictions on converting Pesos to US Dollars, many export taxes and restrictions have also been eliminated.
Read more »By GOFB on Wednesday, November 18th, 2015 in Issue 3 - 2015, Nutrition No Comments
Many fresh foods, especially colourful fruit and vegetables, contain vitamins and minerals that are necessary for body and mind health, and to protect against the ravages of disease and ageing.
Read more »By GOFB on Sunday, September 20th, 2015 in Issue 2 - 2015, Nutrition No Comments
A high level of low density lipoproteins (LDL) could lead to cardiovascular disease, especially in the absence of balanced nutrition and general neglect of health. Fatty plaques accumulate around vessels and arteries, and aggravate the condition to the point of no return. However, disaster can be averted by following simple precautions for a healthy lifestyle.
Calculating the body mass index (BMI) has become a well-known tool in measuring the impact of dietary changes and determining the risk of heart disease. However, the waist circumference is a more effective indicator of cardiovascular risks. Knowing the BMI, measuring the waist, and regularly checking the weight will help in warning of a high cholesterol level.

| In children | Fats accumulate in the intima but the phenomenon is quite natural; this is why children are usually considered out of danger. (The vessel walls comprise three layer : Intima, Media and Adventitia.) |
| In women | Hormones have a protective role until menopause. This explains the reason for the high probability of arterial inflammation or angina in women after the age of 50. |
| In men | Problems arise early depending on personal lifestyle and genetic history. |
Normal weight is between 19 and 25. It is natural for the BMI to increase with age even though the person is following the same dietary pattern. When the BMI is less than 18, it is in the underweight category and the risk of anorexia is increased. When the BMI is more than 25, it is in the overweight category and may lead to obesity. The waist circumference should not exceed 80cm for women and 102cm for men.
We often notice high cholesterol levels in those over 50 years old, but this may affect younger persons as well. Some people suffer from obesity or hypercholesterolemia due to heredity. It is necessary to inform the doctor about the family health history, to help determine what precautionary measures to take. Often, patients are advised to decrease consumption of products with a high glycaemic index. Vegetables, fruit and whole grains have a low glycaemic index, compared to bread, rice, fries and sweets.
Keeping a check on cholesterol
There is no need to apply this evaluation during adolescence, but it is necessary after the age of 40. Based on the test results, the cholesterol level should be monitored every two to three years at least. Patients often refuse to consult their doctor regarding a high cholesterol level, with their main excuse being ‘no time’. However, from the age of 50, it is better for the patient to monitor the basic indicators related to high cholesterol level, as prevention is better than treatment.
Limit intake of saturated fatsThe first step is to be able to differentiate between saturated and unsaturated fats – we tend to name these as ‘bad’ fats or ‘good’ fats. The descriptions are not accurate because extra fats are bad for the body, whether saturated or not. Nevertheless, this doesn’t stop some media outlets and dietitians from encouraging the consumption of ‘good’ fats, meaning unsaturated fats found in oily nuts and fatty fish specifically. Unsaturated fats remain in a liquid state when cooked at a low temperature. Monounsaturated fats lower the LDL (bad) cholesterol level in blood, while polyunsaturated fats work on the total cholesterol level.
Consume omega-3Omega fatty acids help in the functioning of the vascular and cardiac systems, as well as protect them. As the body cannot make omega fatty acids, these must come from food sources. The fatty acids include not only omega-3, but also omega-6 and omega-9 found in some oils such as sunflower oil and soybean oil. One problem today is that the nutritional pattern lacks essential fatty acids. The consumption of sardines, walnuts and almonds has decreased, while fresh fish has become quite expensive.
Eat fruit and vegetablesThose who have a high cholesterol level are advised to maintain a balanced diet. This should include fruit and vegetables as these are rich in vitamins, minerals and antioxidants, and therefore have a role in preventing the formation of fatty plaques on the walls of vessels. Studies have showed that the lack of certain substances enhances LDL oxidation – for example, a deficit in Vitamins C and E, polyphenols found in fruits and vegetables, dietary plant fibres and calcium.
Get regular exerciseTo boost the effect of the new nutritional pattern, add physical activity. This will help decrease the LDL level and increase the level of high density lipoprotein (HDL) or ‘good’ cholesterol. Create an exercise programme that takes into consideration your age and general health status, and which keeps you motivated to work out. If you have not been active, begin slowly and increase the intensity gradually.
Drink sufficient waterHydrating the body will revitalise it and help in maintaining a perfect weight. Doctors recommend drinking 1.5-2 litres of water per day. You can substitute part of the intake with healthy liquids like green tea or fresh juices.
Control blood pressureHypertension increases the risk of myocardial infarction. Visiting the doctor is a way to have peace of mind. Beverages that act as stimulants (coffee, tea or energy drinks) can increase blood pressure, as does salt. So, reduce intake.

Smoking is bad for health in general, and also increases the LDL cholesterol level. Smokers should stop this habit early. Often, cessation will make the body gain weight. A suitable diet and routine exercise will help.
Boost vitamins after menopauseThe dietary pattern usually provides all the nutrients needed by the body. However, the body may not get enough of some essential nutrients in some situations. In women, this becomes obvious after menopause. Without the protective effect of hormones, it is common for women to experience a lack of iron and Vitamin D, for instance. This is not dangerous but we recommend a general check-up after the first blood analysis following menopause.
Maintain the dietSome will find it easy to commit to a particular diet or weight maintenance programme, while others find it an ordeal. Ask for help where necessary. Note that emotional trauma can be translated in the body by an increase or a decrease in weight. Those with hypercholesterolemia will have to keep to a steady and balanced nutritional pattern for life.
It is normal to experience overeating at some point. Carefully control intake, especially during festive occasions when food is abundant. Losing weight becomes very hard especially after a certain age. Eat what you like from time to time but try to lose the extra weight quickly, either through exercise or by avoiding certain kinds of food or decreasing the amount consumed.
Source: Health & Nutrition Magazine,
Issue 170 – October 2014 This is an edited version of the article.